 Hemmroid surgery
Hemmroid surgery, or
hemmroidectomy, is a surgical procedure to remove
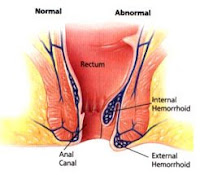
hemmroids. Hemmroids occur when an increase of pressure in the veins around the anus and rectum causes them to become swollen and stretched. They may result from a number of factors such as straining during a bowel movement , pregnancy, prolong sitting, overweight, chonic constipation and a like.
In
hemmroid surgery, hemmroidal tissue and excess tissue around the anal canal is surgically removed (excised). The procedure is typically performed in a hospital or surgery center by a surgeon who specializes in colon and rectum surgeries. An overnight hospital stay is usually required, but in some cases the procedure may be performed on an outpatient basis.
Hemmroidectomy is highly effective, but recovery is similar to recovery from other surgeries and may be initially painful.
Hemmroidectomy is important in the treatment of extensive or severe hemmroids. It can be used in the treatment of both
internal hemmroids and
external hemmroids, as well as those that occur both internally and externally at the same time. It is not generally used for mild- to-moderate hemmroids. However, it may be used to treat less severe hemmroids if other treatment options (e.g., stool softeners, sitz baths) fail.
Hemmroidectomy is also useful in the treatment of patients who have developed certain complications. Persistent bleeding may only be effectively treated with the removal of the hemmroids, although less severe bleeding can be treated with other therapies. When blood clots form inside hemmroids, the hemmroids must usually be removed.
Recovery from hemmroidectomy generally takes between two and three weeks. The risk of
hemmroid recurrence is much lower with hemmroidectomy than with other methods of
hemmroid treatment.
Pain and discomfort are common following
hemmroid surgery and pain-relief medications are usually prescribed. After surgery, the rectal area is monitored for bleeding and laxatives are used to ease defecation. Fluid intake is also monitored. Any increased rectal bleeding, pus drainage, fever, constipation or rectal spasms need to be reported to a physician. It is important to prevent constipation following surgery. Therefore, patients may be encouraged to exercise, drink plenty of fluids and eat a high-fiber diet .
Hemmroid surgery is the most effective treatment for hemmroids. However, it does pose potential risks. Urinary retention, urinary tract infections , fecal impaction and bleeding are the most common complications of the procedure. Alternatives to hemmroid surgery include many minimally invasive techniques, especially
rubber band ligation and
coagulation (e.g., infrared coagulation, electrocoagulation). New techniques for treating hemmroids are also being developed.
Before
hemmroid surgery, the physician will explain the procedure and answer any questions the patient may have. The patient will then be instructed to sign an informed consent form.
The patient will typically be placed on a special, low-residue diet for several days prior to the surgery. A low-residue diet contains very few foods that can become caught in the colon. This helps keep the colon clean for the surgery. The patient’s
hemmroids will be evaluated. External hemmroids will be examined, with particular attention to size, evidence of bleeding and the presence of drainage. Stool softeners and an enema may be used just before the surgery to prepare the bowels. The rectal area will then be cleansed. This may involve a sitz bath, in which the patient sits in a small amount of warm water. After it has been cleansed, the rectal area may be shaved.
Hemmroid surgery procedureHemmroid surgery is performed with the patient under anesthesia. In most cases, a general or spinal anesthetic is used. General anesthetics cause a patient to lose consciousness and sensation by an injection of medication or breathing a medicinal gas. Spinal anesthetics cause a patient to lose sensation of pain by injecting a medication into the area around the spinal cord. Some patients may be able to tolerate a local anesthetic combined with sedation. This causes a loss of sensation in only a specific region of the body. When spinal anesthetics or local anesthetics are used, the patient remains conscious during the procedure.
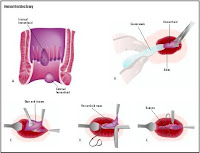
During
hemmroid surgery, an anoscope is used to view the hemmroid and surrounding tissue. An anoscope is a short, rigid tube that is inserted into the anus. Once the surgeon can see the base of the hemmroid, its blood supply is tied off with surgical stitches (sutures). The hemmroidal tissue is removed, or excised, and some of the surrounding tissue is usually removed as well. The surgeon takes care to avoid damaging the anal sphincter. The actual removal of tissue may be done with a scalpel, scissors, cautery (uses an instrument that relies on heat or electricity to cut tissue) or laser.
The edges of the anal or rectal lining (rectal mucosa) around the excised tissue may be left open, closed or partially closed. This is a matter of physician preference. Results and post-surgical pain are similar whether the lining is left open or closed.
After hemmroid surgeryLike with many surgical procedures, pain and discomfort are common following a
hemmroid surgery. However, medications are prescribed to relieve the pain and Sitz baths may be used to relieve discomfort and promote healing.
The patient’s vital signs are monitored regularly during the period immediately after the
hemmroid surgery. The rectal area is monitored hourly for bleeding. Any excessive bleeding is treated. This may be accomplished by inserting a balloon-tipped catheter into the rectum. The balloon tip places pressure on the bleeding area, stopping the bleeding. Prescription ointments may be applied to the rectal area to help it heal and to relieve pain. Dressings, typically pads, are changed frequently.
Stool softeners and bulk laxatives are prescribed to ease defecation. It is important to increase fluid intake while taking these medications. The patient’s fluid balance is monitored. Health care professionals will keep track of how much liquid the patient consumes and ensure that the patient urinates between eight to 12 hours after the surgery.
Patients may be discharged following the
hemmroid surgery or may need to remain in the hospital overnight. It is important for patients to change positions frequently after the procedure, and to lie down for about 15 minutes every hour. This helps to reduce rectal swelling. A special pad is typically given to the patient to ease discomfort when sitting. However, rubber rings are not recommended as they can block blood flow and cause swelling.
Any increased rectal bleeding, pus drainage, fever, constipation, severe abdominal pain, rectal spasms, swelling, weakness or infection need to be reported to a physician. It is also important to keep the rectal area clean. The rectal area needs to be cleansed gently with warm water and mild soap. It should be rinsed thoroughly and gently patted dry.
Patients are urged not to strain during a bowel movement.
Constipation can be prevented with regular exercise and by drinking plenty of fluids and eating plenty of high-fiber foods (e.g., fruits, vegetables). Bulk laxatives may also be used as needed. However, overuse of stool softeners should be avoided. Firm stool is important to dilate the anal canal and prevent strictures (narrowing).
Hemmroid benefits and risksHemmroid surgery (
hemmroidectomy) is the most effective treatment for hemmroids. It frequently eliminates hemmroids with no recurring symptoms. When symptoms do recur, they are rarely severe enough to require additional surgery. However,
hemmroidectomy does pose certain risks. Complications can be minimized with proper surgical technique during the procedure and adequate pain control, attention to fluid intake and proper use of bulking laxatives and stool softeners after the surgery. Patients are urged to discuss the use of laxatives with their physicians. Complications of hemmroidectomy may include:
•
Pain. Pain is very common following
hemmroid surgery, as with many other surgeries. The degree of pain varies between patients. Pain relievers are administered to relieve pain.
•
Urinary retention. Difficulty emptying the bladder. This temporary complication may occur, depending upon several factors. These include the amount of fluids given during and after surgery, the degree of pain the patient experiences and whether the patient has a history of difficulty emptying the bladder. In some cases, patients may require a catheter to drain the bladder. The need for catheterization can be reduced by limiting fluid intake and using pain medications and warm sitz baths. A physician will be able to determine the risk of this complication and suggest proper levels of fluid intake and other prevention and treatment measures.
•
Urinary tract infections. These occur in some patients and may be a result of urinary retention.
•
Fecal impaction. A mass of hardened feces becomes lodged in the rectum. This may be due to the pain following surgery, which worsens with defecation. This may cause patients to hold in their stool to lessen their pain. Holding in stool is a common cause of fecal impaction. The use of narcotic pain relievers may also be a factor. Bulk fiber, stool softeners and stimulant laxatives are generally effective in preventing fecal impaction. In some cases, fecal impaction may require manual removal while the patient is anesthetized.
•
Delayed bleeding. A few patients may experience bleeding seven to 16 days after hemmroid surgery. It is generally believed to be caused by the shedding of tissue that has been operated on and tends to require closing with stitches.
•
Anal stenosis. Narrowing of the anal canal. This is a long-term complication. It may result from the removal of too much tissue around the hemmroids.
•
Submucosal abscess. An infection of the tissue just below the anal or rectal lining, resulting in an abscess (a collection of pus). This is a very rare complication that, even more rarely, can result in death.
In addition, hemmroidectomy carries the risks common to all surgeries including bleeding, skin infection and allergic reaction to anesthesia.
However,
hemmroid surgery is not always an option. For example, it is not used in patients with Crohn's disease of the rectum, which is a form of inflammatory bowel disease. In this condition, the intestinal tract is easily irritated. Hemmroid surgery on a patient with Crohn’s disease is much more likely to cause serious complications. In cases such as these, the risks of hemmroid surgery outweigh the benefits.
 Hemmroid removal is only recommended when your hemmroid is already in severe stage. Hemmroid removal is performed via the standard form of hemmroids surgery called Hemmroidectomy. This type of hemmroid surgery is performed in cases of large internal hemmroids, large external hemmroids, and hemmroids that have not been treated effectively by other methods. Although most hemmroids are treated by medicines and other different remedies to provide relief from the disturbing symptoms of pain and inflammation caused by the affected rectal tissues, severe cases of the hemmroids requires hemmroid removal if you want long-term hemmroid relief.
Hemmroid removal is only recommended when your hemmroid is already in severe stage. Hemmroid removal is performed via the standard form of hemmroids surgery called Hemmroidectomy. This type of hemmroid surgery is performed in cases of large internal hemmroids, large external hemmroids, and hemmroids that have not been treated effectively by other methods. Although most hemmroids are treated by medicines and other different remedies to provide relief from the disturbing symptoms of pain and inflammation caused by the affected rectal tissues, severe cases of the hemmroids requires hemmroid removal if you want long-term hemmroid relief.